


Diabetes experts and leading organisations such as Diabetes Australia, the National Diabetes Services Scheme (NDSS), the ADA and EASD 2021 Consensus1-8 recommend that people with type 1 diabetes using continuous glucose monitoring (CGM) should also have access to a blood glucose montitor (BGM), in several situations:
Before meals to give you a chance to adjust the meal insulin dose
If there are concerns that CGM readings do not reflect your blood glucose
To detect hypoglycaemia in situations, such as:
People with diabetes, especially those on insulin therapy, have to regularly check their glucose (sugar) levels. There are different types of glucose monitoring systems available for people with diabetes:9,10
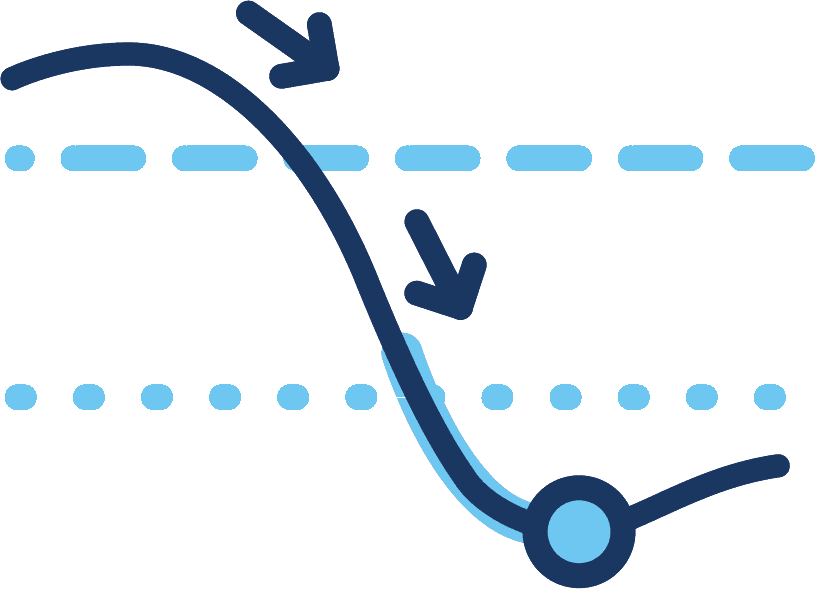
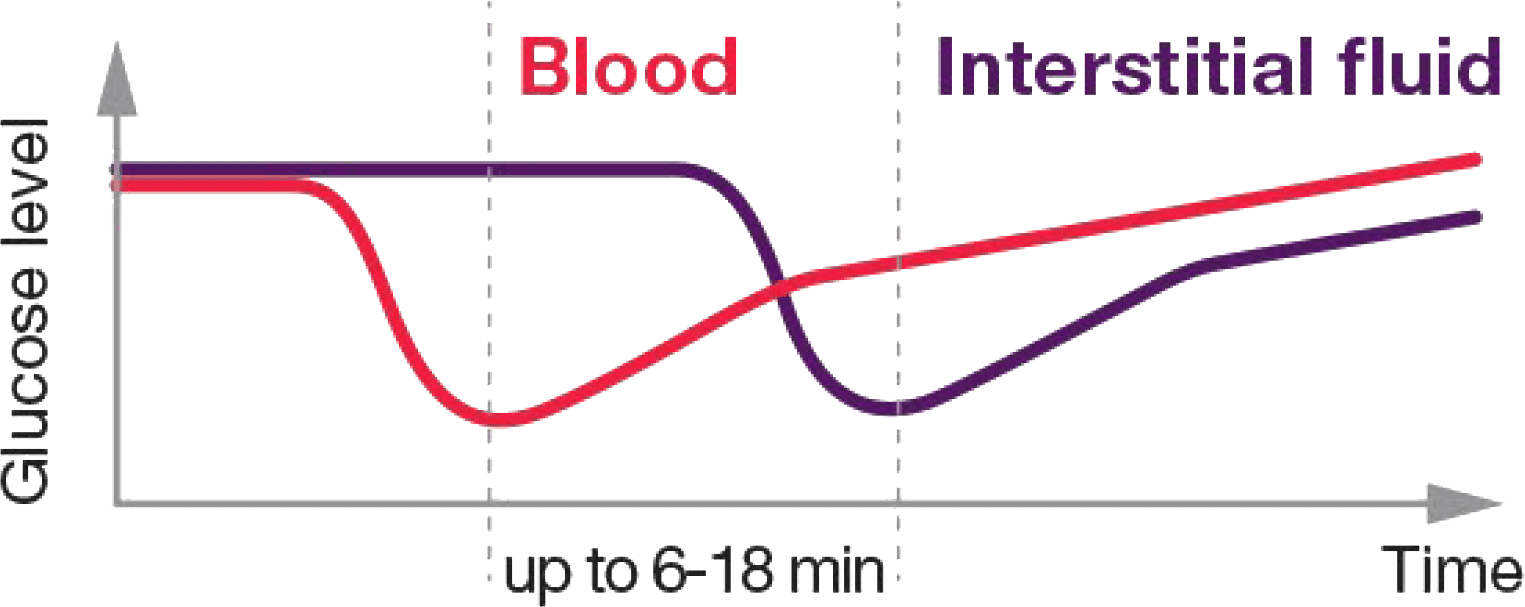
Blood and IF glucose values are not equivalent, and it can take up to 6 to 18 minutes for IF values measured by a CGM to reflect the levels of glucose in the blood. This means you may be making decisions based on old information.11
The accuracy of CGM systems can also vary significantly throughout the day, due to the activities of daily life.12 This is why CGM manufacturers state that everyone using their systems should also have access to BGM.1-8
Routine calibration

When taking paracetamol
Closed loop diagnostics

When waiting on supplies

When symptoms do not match readings
Rapid rates-of-change
No value or trend arrow

Any time accuracy is in question
Dosing insulin

Day one of sensor use

Transmission issues

Recovery from hypoglycaemia
If you are pregnant, BGM is strongly recommended if you have pre-existing diabetes or develop a form of diabetes during pregnancy known as gestational diabetes mellitus, to achieve the best glucose levels.13
Ask your doctor about the target ranges you should be aiming for.
^ Terms and conditions apply: Upgrades to CONTOUR®NEXT are limited to one (1) per NDSS registrant in an 18-month period. Requests for more than one meter in this period may not be accepted at the sole discretion of Ascensia Diabetes Care. Please contact our local customer service team on 1800 289 312 if you have a request outside of these guidelines.
* Minimum accuracy requirements of ISO15197: 2013 Section 6.3 standard require ≥95% of the measured values to fall within ±0.83 mmol/L at glucose concentrations<5.5 mmol/L or within ±15% at glucose concentrations ≥5.5 mmol/L compared to the reference method.
† An ad hoc analysis demonstrated that 95% of the results were within the error range ±0.3 mmol/L or ±5.3% of the laboratory reference values for glucose concentrations <5.5 mmol/L or ≥5.5 mmol/L, respectively.
1. Diabetes Australia: Blood glucose monitoring | Diabetes Australia. Accessed May 2023
2. NDSS Continuous Glucose Monitoring Factsheet: Version 7 June 2022. First published April 2018. NDSSFS010. Continuous glucose monitoring fact sheet (ndss.com.au)
3. American Diabetes Association. 7. Diabetes Technology: Standards of Medical Care in Diabetes. Diabetes Care. 2022;45(Suppl 1):S97–S112.
4. Holt RIG et al. Diabetes Care. 2021;44(11):2589–2625.
5. Medtronic Guardian Connect with Guardian Sensor 3 User Guide. Printed in Australia 02/2018.
6. Abbott FreeStyle Libre 2 User Manual, ART43974_rev-A_02/21
7. Dexcom G6 CGMS User Guide LBL014003 Rev 008 MT23976, 2018.
8. Dexcom G5 Mobile User Guide LBL013445 Rev 005 MT23435, 2017.
9. Freckmann G et al. J Diabetes Sci Technol. 2019;13(3):575–583.
10. Richardson & Shaginian. Hypoglycemia Detection in Diabetes. 2022.
11. Choudhary P et al. Diabetes Technol Ther. 2011;13(11):1121-1127.
12. Pleus S et al. J Diabetes Sci Technol. 2021;1932296821992373.
13. American Diabetes Association. Section 15. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes. 2022. 2022;45(Suppl 1):S232–S243.
14. Pleus S et.al, User Performance Evaluation and System Accuracy Assessment of Four Blood Glucose Monitoring Systems With Color Coding of Measurement Results. J Diabetes Sci Technol. 2022 Nov 26:19322968221141926. doi: 10.1177/19322968221141926.